Heart valve operations may not be necessary in the future
Xeltis develops 'living' heart valves made from biodegradable polymers. This technology may make a whole range of heart valve operations redundant in the future.
Heart and soul
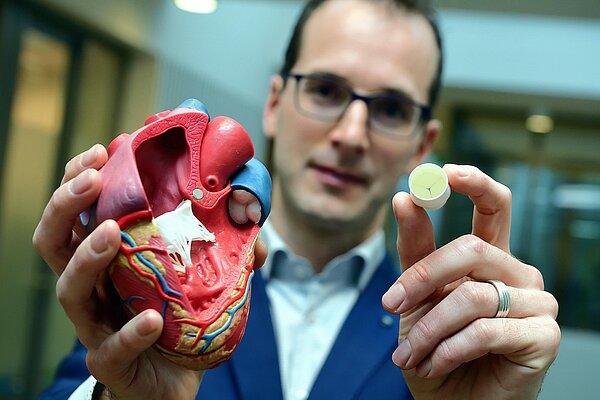
He is co-founder of Xeltis. A spin-off from research performed by TU Eindhoven and one of the most promising start-ups in the medical technology field in the world. The company develops 'living' heart valves made from biodegradable polymers. This technology may make a whole range of heart valve operations redundant in the future. This will be a godsend for children in particular. So what drives Martijn Cox? “I try to understand things completely through a learning process and only stop when I am satisfied that I have achieved that objective. Giving up is not in my nature.”
A patient is about to be given 'his' plastic heart valve on that day in Budapest . This is the much-anticipated culminating moment after 12 years of research. Martijn Cox has been given permission to watch the surgeon from inside the operating theatre. A little weak at the knees, he closely observes the surgeon’s operating technique. “The operation went perfectly - as you would expect of such an experienced surgeon. Even so, it was still a weird and special feeling, incredibly exciting. From the very beginning, your dream has been to develop a biodegradable plastic heart valve. But obviously it has to work.” Then: "Yes, the patient is doing well. Just like all the other children who are now equipped with our heart valve. But we are not there yet. We still have many avenues to explore.”
Budel
Martijn Cox is the Chief Technology Officer of Xeltis. A company that is seen worldwide as one of the most promising medical technology start-ups ever. The people of the company are working on a revolutionary innovation that literally makes your heart beat faster. A plastic heart valve that automatically undergoes a transformation in the patient’s body to become a living heart valve. Cox is aware of the glowing reviews, but simply shrugs his shoulders. That must be the down-to-earth Brabander in him. He grew up in the village of Budel, and now lives there again, on a plot of land where his grandfather's cows once grazed. His wife comes from Bergeijk, a stone's throw away. “I lived in Eindhoven for a while, but Budel is my home. That’s where my family and friends are. Budel reflects who I am. I value my roots.”
Chess grandmasters
He comes across as a slightly shy, diffident person. He used to be described as “a quiet boy and a bit withdrawn.” He likes outdoor sports and is a good chess player. His father taught him the basics of chess: “When he couldn't beat me anymore, he sent me to a chess club.” He occasionally defeated boys who are now grandmasters, but in spite of his talent, his real ambitions lay elsewhere. In his first year at secondary school, he already knew what he wanted to do: study biomedical technology at Eindhoven University of Technology. A new course at the time. “I was one of the students in the third intake year.” He is good at science and loves biology; this course combines both. Other options, like studying to become a doctor or pharmacist, did not appeal to him. “I hate learning things by heart. I am far too lazy for all that effort. Learning rows of words doesn’t inspire me at all. I don't want to learn things blindly, I need to understand what I learn. And I keep at it until I understand something completely. Giving up is not in my nature.”
The human body and technology
For those unfamiliar with this discipline: biomedical technology is a collective term for developments in biomedical science and technology. It interfaces with physics, chemistry, electrical engineering, computer science, mechanical engineering, biology and physiology. Biomedical engineers try to understand diseases and develop equipment to diagnose and treat them. Bioprocess technology in Wageningen is a similar course, says Cox. “But that course focuses more on nutrition. I am more interested in the human body. I want to know how it works and how you can unravel and, where necessary, improve how the body functions. You can design all kinds of mathematical and chemical models for this.”
Internal combustion engine
A human being expressed as a mathematical formula? That requires some explanation. Cox: “Our body is a combustion engine that burns proteins and carbohydrates. Both give you energy. You can very accurately calculate how much fuel you need for excellent performance during a sporting event at world-class level.” Just think of cyclists, long-distance skaters and marathon runners. Even though he competes in half-marathons, he doesn’t use his arithmetical skills to check whether he has eaten enough. “Chemistry lets you analyse diseases extremely accurately. When you know which proteins play a crucial role in disease processes, you can create molecules that either inhibit or activate production of those proteins. And use that knowledge to produce medicines.”
Meaningful and impactful
Orthoses, prostheses, a pacemaker, an artificial intraocular lens and (computer) equipment used in surgical procedures: these are just a few examples of ground-breaking achievements in biomedical technology. During his course in biomedical technology, Cox soon became fascinated by artificial heart valves; a line of research that is being pursued in Eindhoven and at other universities. “Developing a heart valve gives me greater satisfaction than developing a new kind of vacuum cleaner. The heart also appeals to me more than a knee. That has nothing to do with complexity, because a knee is perhaps even more intricately constructed. But the impact is greater. That's part of my character. I want to do things that are meaningful and that have an impact.”
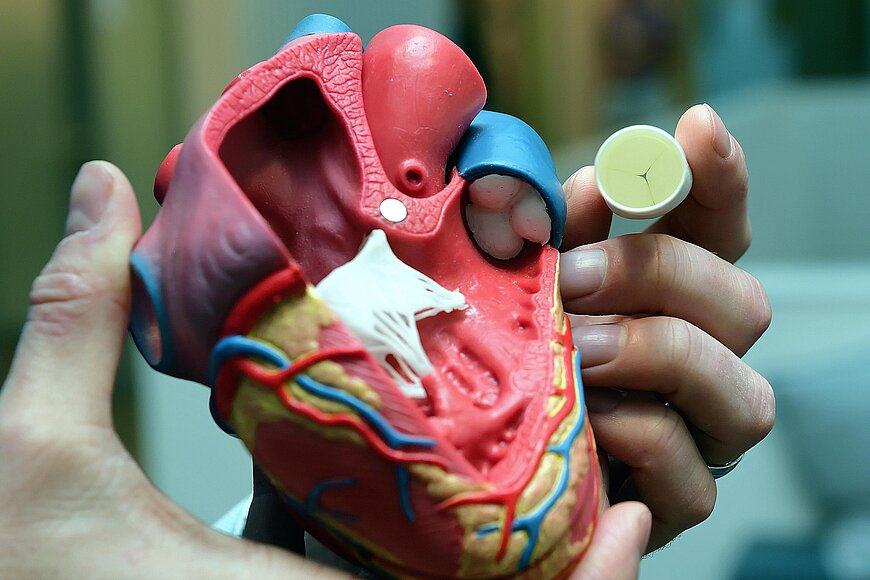
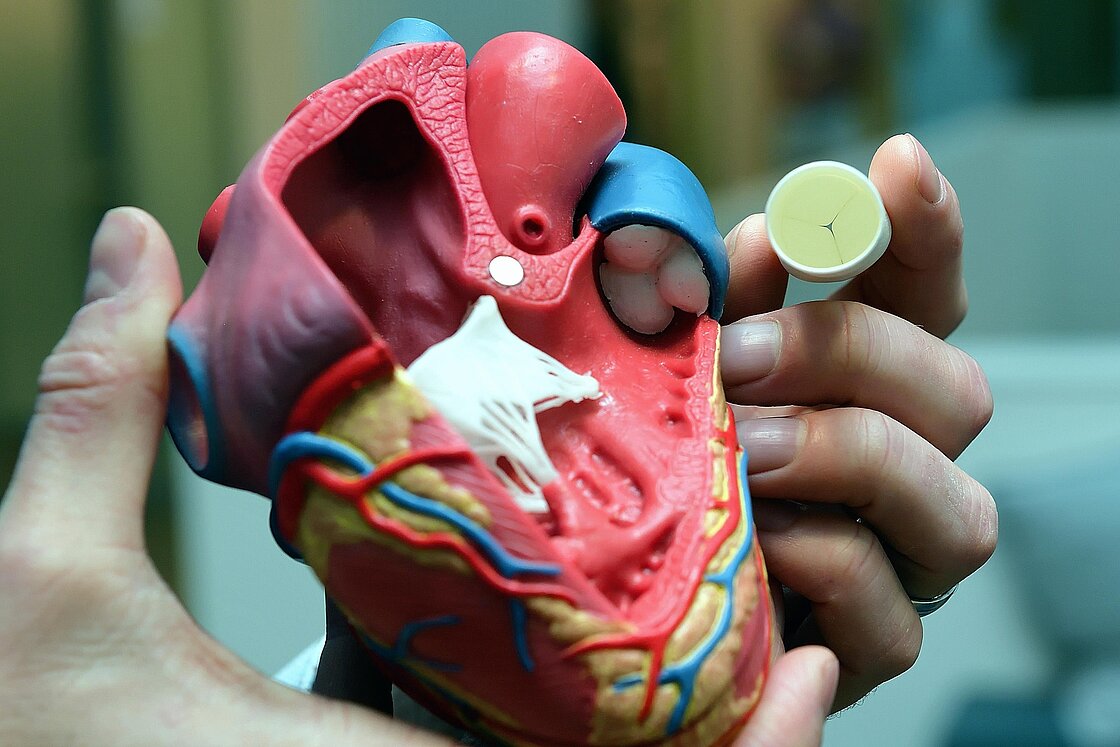
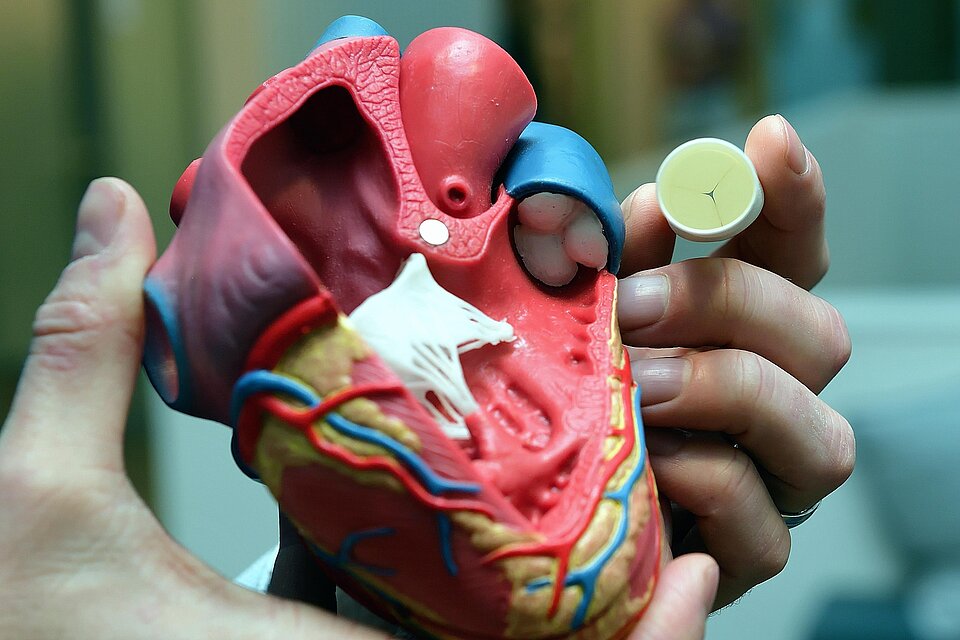
Open your heart
It's time to look at the inside of the human heart. Cox picks up a model, puts it on the table and immediately start to break it down into its component parts. A heart consists of a left and right half, he tells me, and each half has an atrium and a ventricle. Each half also has two heart valves. They act in unison to ensure that the blood flows through your body in the right direction. The left half of the heart (with the aortic and mitral valve) pumps the blood towards the tissues and organs, the right half (with the pulmonary and tricuspid valve) pumps it towards the lungs. And the whole set-up is quite unusual: “The heart valves play an important role in the bloodstream even though they have no mechanism for active movement. They have no muscle cells and move synchronously with the flow of blood. Pressure differences cause them to open and close.” Heart valve disease or some other abnormality, often attributable to illness or age, can cause a heart valve to leak. In such cases, the valve has weakened, stretched, suffered damage or narrowed. As a result, less blood passes through the valve, or some of the blood flows back into the heart. Cox: “So the heart has to work harder to pump enough blood through the body.”
Children
In industrialised countries, about 2% of the population is affected by heart disease. Hundreds of thousands of patients undergo heart valve surgery every year - 5000 in our country. As many as 80,000 children worldwide, and perhaps even more, are born every year with a failing pulmonary heart valve, the valve between the heart and lungs. “These infants sometimes have to undergo three to five major surgical procedures. Procedures that are not only stressful, they are also expensive and not devoid of danger. Furthermore, they also have to take anticoagulant drugs for the rest of their lives.”
Biodegradable plastic heart valve
There had to be a solution, he thought. The idea: a plastic biodegradable heart valve that 'trains' cardiac cells to reproduce and make their own heart valve tissue and then disappears automatically, leaving behind a mature and living valve made from the body’s own tissues. Cox: “In the first instance, we removed cells from a patient in order to grow the valve. We placed them in a mould, shaped to replicate a heart valve, and then used a bioreactor to kick-start them into developing into a large and strong tissue mass. Next, you implant the mould in a patient. But that method turned out to be expensive and complex.” Fortunately, he was able to stay on at TU/e after he graduated. He and other PhD students embarked on an intensive heart valve research programme. “I wanted to understand more.” He is fond of quoting Nietzsche: ‘What doesn't kill you, makes you stronger’. “If you understand your failures, you can avoid them the next time round. You learn more from one failed experiment than from ten that go without a hitch.”
QTIS/e
His PhD research at TU/e focused on new ways of measuring the strength of tissues. As his work progressed, he started to ask himself: ‘What if I were to start my own business. Do I have the knowledge and skills?’ He enrolled for various business-related courses. It was at Milan airport, after a trip to the Italian Alps with colleagues, that his professor casually mentioned that the department had received a government grant for starting up a business. A spin-off to take the research to the next level and develop a product. “My immediate thought was, I need to ask him for a lift.” And his initiative was rewarded. So QTIS/e, or Quality Tissue Engineering, was established in 2007. “The forward slash with the lower case e is a reference to the University of Eindhoven.”
Xeltis
Three years later: he has completed his PhD research and a two-year Master degree in Business Innovation, and QTIS/e now employs twelve people. And then a new opportunity comes knocking on his door. Xeltis from Switzerland, a spin-off from the University of Zurich. That company also focuses on the development of a plastic heart valve. Cox: “They were strong in business development, had more commercial people. We were more active in research.” A perfect match. Complementary to each other rather than competitors. The R&D lab stayed in Eindhoven, while the head office moved to Zurich. “They were closer to our Swiss investors there.”


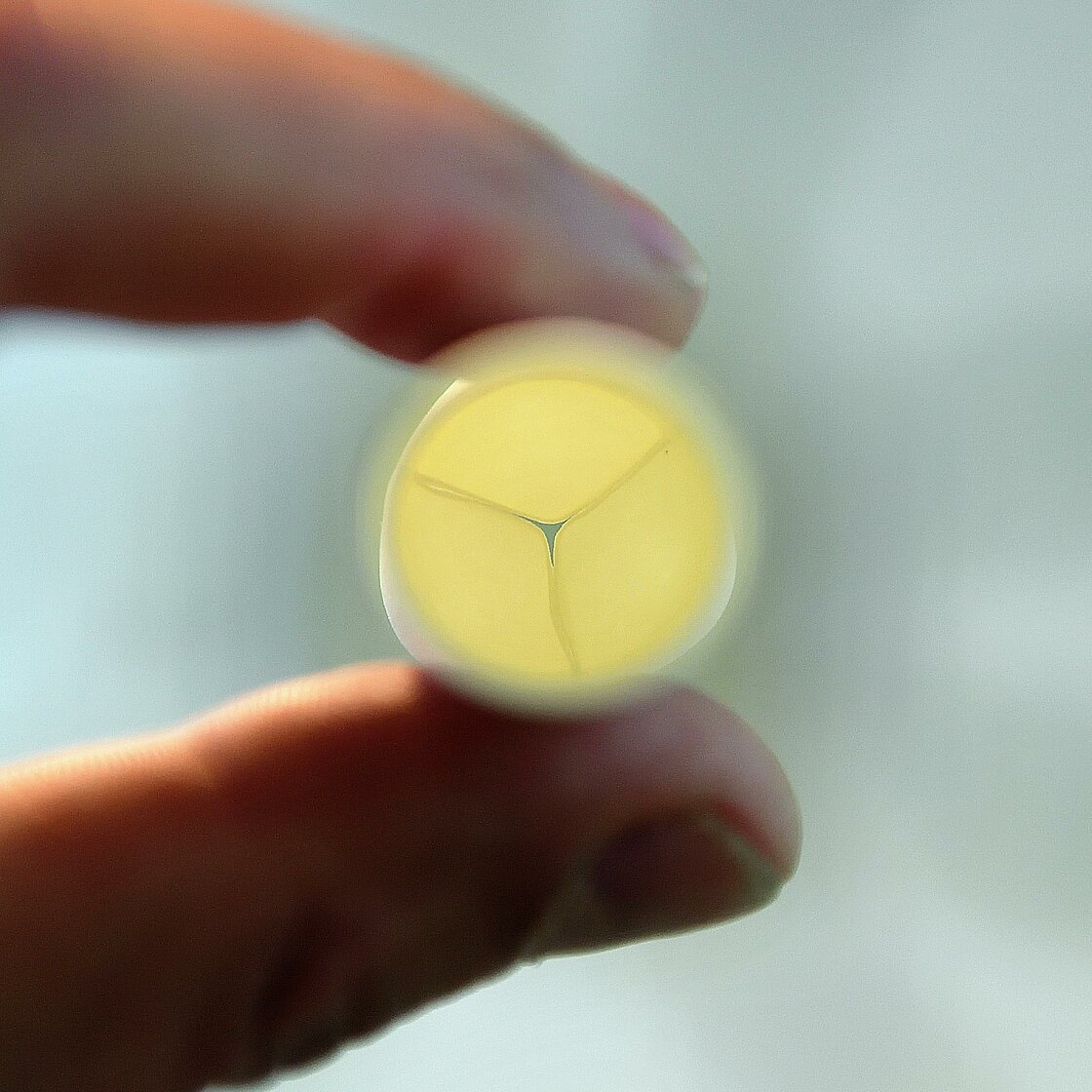
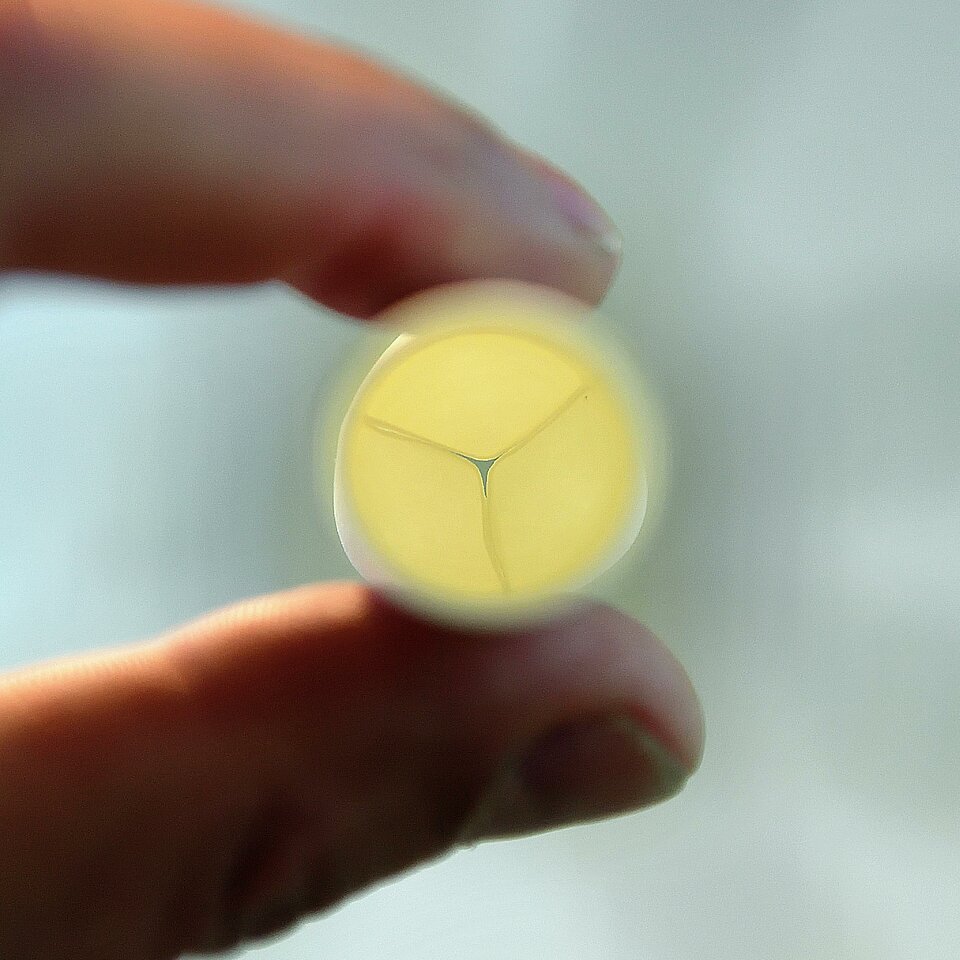
Tube with a Mercedes logo
Five people still work from the head office in Zurich. The lab in Eindhoven has increased in size: 50 people continue to work on a plastic heart valve. Which already exists. He gives me one. An innocent looking tube, about 17 millimetres in diameter and as light as a feather. In the middle, you can see a ring of what look like nail-tip indentations. Sinuses, if you want to use the correct term. In the same area, you can see a closure on the inside, consisting of three membranes adjacent to each other, just like a Mercedes logo. The exact shape of a human heart valve, says Cox. Give it a squeeze, he says encouragingly. And you see the closure open automatically and then close again. “Blood can be pumped upwards through the valve because the membranes open, but not in the other direction because the membranes seal against their seats.”
Supramolecular polymer
The tube feels like paper, but be careful what you say. “Paper? Don’t be irreverent.” The ‘paper’ is in fact a biodegradable polymer, also developed in Eindhoven. It is officially known as a supramolecular polymer. The result of research carried out by French chemist, Jean-Marie Lehn, and two American chemists, Donald Cram and Charles Pederson. The development of supramolecular chemistry earned that star trio the 1987 Nobel Prize for Chemistry. A professor at TU/e has taken their original invention and developed it further. And now it serves as the basic material for the revolutionary biodegradable heart valve. Cox: “When the French chemist heard how we had applied his invention, he immediately wanted to join the Advisory Board.”
Yarn
They melt the Nobel prize-winning polymer down at Xeltis. Then they produce super-thin threads of the material, even thinner than a human hair, in an electro spinning process. This yarn is used to produce the tube. Cox is vague about the exact amount of yarn required to produce a tube. But you can assume that it is in the order of a number of kilometres, he says with a broad smile. “You can't see it with your naked eye, but the material has a porous open structure. This structure provides enough space for cells from the blood stream to reproduce and generate new heart valve tissue. The artificial valve is like a skilled mechanic who repairs his own faulty heart valve. You can compare it to a cut on your finger. That also repairs itself without leaving a scar.
Pulmonary valve
At the end of 2016, a total of twelve children from Switzerland, Poland, Hungary and Malaysia received a new pulmonary valve. This is the valve between the right ventricle of the heart and the pulmonary artery. Its job is to ensure that no blood flows back into the heart. Recently, a further study started in America where another 10 children will receive an Xeltis implant. Cox: “Children are our main focus at this early stage. They stand to benefit most from growing a natural new heart valve. They also experience more problems with artificial valves than adults. So their need is greater and the risks are smaller. Thanks to our artificial valve, they may only need to undergo surgery once, and there is a good possibility that they will never again have to take medication for their condition.”
Aortic valve
Once the Xeltis heart valve has been proven a success for children, a version for adults will follow. With a larger diameter. This explains why the people at Xeltis are now focusing their development efforts on an artificial aortic valve. A development that will also require several years of research. The shape, the thickness, the implementation method: each valve looks slightly different and has a slightly different function. Cox: “We know that tissue forms, and we know what kind of tissue it is, but we do not yet sufficiently understand when and why a particular tissue forms there, and where variations come from.” And no researcher likes variations. “Obviously, each individual is different, but perhaps we can discover a pattern, and then translate that pattern into mathematical models and a measuring method so that we can learn to understand the process and the mechanisms even better. We still have some way to go before we have a complete solution.”
45 million
One thing is certain: investors love Xeltis. Last year, they were good for another investment of 45 million euros, the largest amount raised in that year for a privately owned European medical device company. In 2014 and 2015, the medical technology start-up raised 57 million euros. Money that is badly needed to perfect the product and take on more employees, says Cox. “We are investigating how the heart valve, folded into a thin tube, can be inserted into an adult patient via the groin. When it reaches its destination, it unfolds with the aid of metal springs. If successful, this will eliminate the need for open-heart surgery.”
Proud
Even so, the heart valve may never actually make it to the market. An invention that can help tens of thousands of people each year and reduce complications, repeat operations and healthcare costs, not to mention the benefits for all those babies born with a heart valve defect. This is mainly because European legislation is becoming increasingly strict. And also partly the result of breast implantation scandals, Cox says. “We are working on a complex and new product. In both a technical and legal sense.” He is convinced that everything will work out. All the signals are positive. “Everybody who works here feels good about what we do. It is a meaningful product. It has a huge impact on people's lives, improves their quality of life. Being involved in this initiative makes you proud, it makes every employee proud. Everyone reacts enthusiastically when we tell them about our work. That motivates us even more. And, as you know, giving up is not in my nature.” With a meaningful look, he says: "What doesn't kill you, makes you stronger.”