Startup AquaWomb gives premature babies a better start

Researchers from TU/e, Máxima MC, and The Gate are setting up a company together with TU/e for medical equipment for premature children.
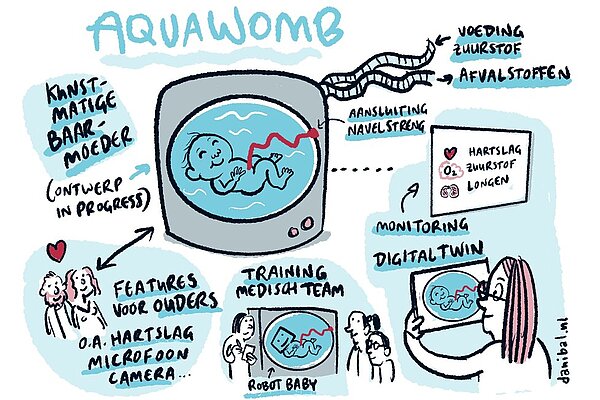
The newly founded start-up AquaWomb is developing a liquid-filled incubator for clinical practice using insights from the Horizon study ‘Perinatal Life Support’. Their dream: to give premature children a better start, by allowing them to develop immersed in amniotic fluid until they are ready to breathe air.
Now that the Horizon study on Perinatal Life Support (PLS) has been completed, a number of researchers are starting follow-up research within the Departments of Biomedical Engineering and Industrial Design.

Researchers Myrthe van der Ven and Guid Oei, together with business developer Marcel Quist, chose a different path. Together with TU/e, they founded the company AquaWomb, with the dream of bringing a working liquid-filled incubator into clinical practice.
Premature children
The company focuses explicitly on the clinical environment where these very premature babies are cared for. In the Netherlands, this is usually done in a NICU (neonatal intensive care unit) - an intensive care unit for very young children.
Before the Aquawomb team can bring a fully functioning liquid-filled incubator to the market, the scientific results must be further developed into a product. To this end, the company expects to run on innovation and research subsidies in the first few years. The roadmap for the development steps of the liquid-filled incubator is made on the basis of customer research that is currently taking place.
The Perinatal Life-support System – the liquid-filled incubator
In the Netherlands, birth care is provided for children from 24 weeks of pregnancy. Thanks to the knowledge and skills of obstetrics-gynecological care in hospitals and at our NICUs, the chances of survival for these children are getting better and better.
However, these children are not yet ready to function outside the womb, i.e. in air. The Horizon-2020 research that has been carried out by TU/e, Máxima MC, Medsim, and Uniklinik RWTH Aachen in recent years aimed to investigate how the care for these children can be improved. Not only to improve the chances of survival, but mainly focused on reducing complications after birth (such as lack of oxygen due to the lungs not yet functioning optimally) and long-term consequences for these children.
To this end, work has been done on a new type of incubator into which the newborn can be transferred directly from the uterus, while being continuously submerged. Such a liquid-filled incubator, which the startup AquaWomb will further develop, should not only ensure that the baby can continue to develop in a safe environment.
It is also important that the caregivers know how the baby is doing and that there is contact with the parents in order to be able to build a bond with their child right from birth. Myrthe van der Ven, researcher and CEO of AquaWomb, and Juliette van Haren, researcher and designer at the Department of Industrial Design, explain how this works in the video from the University of the Netherlands.
Developing the manikin
The first step for AquaWomb is to further develop the special manikin that was developed in the PLS study. ‘Manikin’ is the technical term for a realistic model of the human being, for example, for the training of medical students.
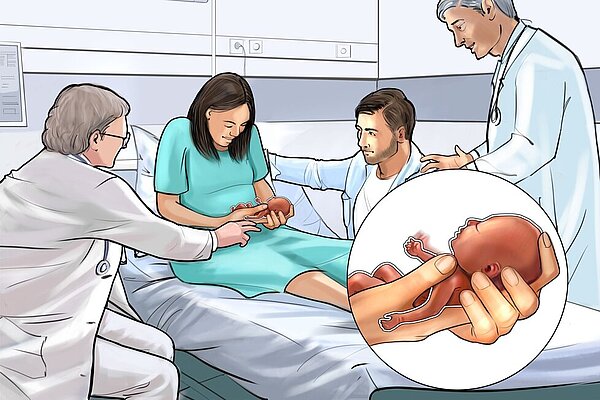
Illustration of how expectant parents can use manikin to get used to caring for a very premature child. Illustration: Aquawomb / Mary-Ann Pepers
In this case, it is a realistic model of a baby born after 24 weeks of pregnancy. Juliette van Haren and her colleagues from the Department of Industrial Design designed this manikin and the first versions of the liquid-filled incubator during her PhD research.
Van der Ven: “The manikin is not only realistic in terms of size and weight, but it also contains sensors. This allows us to measure exactly how the baby is doing, such as oxygen and heart rate, but also brain blood flow and temperature.”
“Digital twin models are linked to the manikin, so that we can realistically estimate whether the baby is doing well during the procedures and treatments. This makes the manikin not only suitable for further research, but also for educating everyone who has to deal with extreme premature birth, from expectant parents to nurses and gynecologists.”
Retrieving user requirements
“Parents who are expecting a premature birth have most likely never seen a premature baby in real life, let alone held it in their hands,” explains Van der Ven. “That's why we think there is a market for the manikin. That is market research that we will start immediately.”
“I am really looking forward to interviewing people about the manikin and thus collecting user requirements for this manikin. We conduct these interviews in Europe because you can see that neonatal care differs quite a bit worldwide. The rules and regulations in Europe are more similar in that respect. We are going to make special demonstration models of the manikin for this research.”
Increasing awareness
As a start-up company, it is always difficult because the target audience of the company does not know you yet. So AquaWomb is also working to increase its awareness. The network of renowned gynaecologist and researcher Guid Oei certainly comes in handy.
“I expect that we will visit many hospitals to consult with their obstetrics and pediatrics teams about their requirements for the liquid-filled incubator,” says Van der Ven. “Conversations with parents of premature children are also on our program.”
“In addition, we know our competition quite well,” explains Van der Ven. “For example, there are teams in the United States, Australia, and Barcelona that are already working on a liquid-filled incubator. They do differ from us in one important way, and that is that they are mainly set up to transfer the neonate with a surgical method rather than obstetrics.”
Those surgical teams are already a bit further along in their development. For example, there are already teams with successful animal experiments, while these experiments are still on the future roadmap at AquaWomb.
Strong story from obstetrics
“The surgical solutions are by definition based on a caesarean section, after which the baby is transferred to the incubator under anesthesia and through the air and connected to all devices. At AquaWomb, we want to stay as close to nature as possible and transfer the baby from a caesarean section via a special transfer bag filled with artificial amniotic fluid into the liquid-filled incubator.”
“In addition, when designing our incubator, we focused not only on medical factors, but also on the ease with which nurses can care for the baby and how parents can bond with their child in the liquid-filled incubator. That really makes our design different.”
In addition, the Aquawomb needs less animal testing thanks to the mathematical models and the test measurements with the manikin. This makes it possible to predict the safety of the child in the liquid-filled incubator and the transfer of the child from the mother to the device very accurately.
“That is why we only need animal testing in the final step as mandatory validation for the medical world. And then we hope that our ambitions will come true: namely, to offer a better start to very premature children.”

